Jim Quigley had been sober for four years and was one semester away from graduating from Bible college when his stopped car was rear-ended by someone going 50 miles an hour.
“I ended up having two artificial discs put into my spine,” he said. He also ended up with a prescription for opiate painkillers.
“I was allowed to have eight pills a day if I took them like the label said,” he said. “But in my mind, if I took all eight at one time but no more, I wasn’t really abusing them.”
A month after surgery, his prescription ran out, and he quit using. But he fell back into alcohol and drug abuse and, three years later, came back to prescription opiates.
“My last year down in Florida, I was in the hospital three different times for pneumonia related to my substance abuse,” Quigley said. “I was an IV drug user. I had used dirty needles, and had cellulitis [skin] infections. I almost lost my hand. I was in three crisis stabilization units for suicide attempts. One time I took so much medication that I was in a coma for four days.”
Quigley’s previous church had a new pastor, and the man prayed for him, let him use the studio apartment behind his house, and gave him a job doing maintenance around the church building.
“About two weeks went by before I finagled a way to get drugs delivered to me,” Quigley said.
Not long after, at 35 years old, Quigley overdosed on opioids and had a heart attack. The worst part: “I was found by [the pastor’s] three small children, lying on the floor of his house in my underwear.”
But Quigley still couldn’t get clean until his cousin found him a long-term rehab place in North Carolina. “They talk about all that God stuff you went to college for, so you might be interested,” she told him.
It wasn’t his first run at rehab, and Quigley was feeling “pretty worn down and beat up.”
His first night at Freedom Farm Ministries, a local pastor told the room, “A lot of you guys have had at one time a relationship with the Lord. You think, I’ve gotten so far away from God, I don’t know how I could ever get back to him. I need to tell you—God hasn’t gone anywhere. You just need to repent.”
“I said the first honest prayer I’ve said in years,” Quigley said. “There were no bolts of lightning. I just asked for help.”
He would go on to graduate from the program, then work his way to up executive director. Today, Quigley works with about 100 addicts a year. He requires his residents read Oswald Chambers each morning, write papers on Tim Keller’s Prodigal God, and take a class on covenant theology. They learn about the medical components of addiction and how to identify triggers. They attend church twice a week, do physical labor, and get random drug tests.
“It’s not all rainbows and unicorns—ultimately, I can’t change anybody,” Quigley said. “I just continue to present the truth to them, and see God grab hold of their lives.”
Freedom Farm is just one way that Christians are tackling the opioid crisis, which killed 33,000 Americans in 2015, up from the record-setting 28,647 in 2014. Thanks to opioids, overdosing on drugs is now the most common cause of death for people younger than 50.
Earlier this month, President Donald Trump declared the opioid crisis a national emergency, in response to a commission report that also called for equipping law enforcement with the overdose-reversing drug naloxone and better tracking of prescription data. In 2010, Americans—which make up less than 5 percent of the world’s population—consumed 80 percent of the world’s opioids and 99 percent of its hydrocodones (semi-synthetic opiates like Vicodin or Lortab).
“America is enduring a death toll equal to September 11th every three weeks,” the report said. “[I]f this scourge has not found you or your family yet, without bold action by everyone it soon will.”
Opiate Origins
Opiates—which include heroin, codeine, and morphine—are drugs made from the opium poppy. When ingested (through snorting, smoking, swallowing, or shooting up), the chemicals attach to receptors in the brain, blocking it from receiving any signals of pain and replacing them with euphoria.
The brain loves this, so it rewards itself with a lot of dopamine, which produces an intense rush of pleasure and the motivation to do it again.
Using opiates to replace pain with pleasure has been around as long as the poppy—ancient Sumerians called it the “joy plant.” It’s been causing trouble almost as long, including two major wars between England and China over whether England could supply China’s opium dens (the British won both times), the addiction of Civil War soldiers to morphine used for injuries, and the invention of a German dilution that was supposed to be less addictive but turned out to be heroin.
The German drug company Bayer introduced heroin to the United States along with aspirin, but wasn’t alone in believing it to be less harmful than it actually was. In the 19th century, opiates were ubiquitous, found in products as common as teething powder, children’s cough syrup, and menstrual cramping relief.
The government attempted to get a handle on things through the 1906 Pure Food and Drug Act (which required labels to note if drugs were “dangerous” or “addictive”), the 1909 Smoking Opium Exclusion Act (which banned the import of recreational opiates), or the 1914 Harrison Narcotics Tax Act (which listed and taxed opium dispensers).
But opiates are really effective (“Morphine is hard to beat,” said one Wake Forest School of Medicine researcher working on an alternative), and pharmaceutical companies kept releasing different variations.
Knowing the addiction risks, many modern doctors were careful with their prescriptions. Eventually, one Boston University doctor grew curious about how many patients actually became addicted to their prescribed narcotics. Herschel Jick and his graduate student Jane Porter sifted through their records and then wrote an ill-fated, five-sentence letter to the editor of the New England Journal of Medicine in 1980. The two reported that less than 1 percent of Boston University Medical Center patients had become addicted to the narcotics they received while in the hospital.
“We conclude that despite the widespread use of narcotic drugs in hospitals, the development of addiction is rare in medical patients with no history of addiction,” they wrote.
They weren’t wrong. Recent studies also show that most patients don’t become addicted, especially if their prescription is for less than a week or if they have no history of addiction.
But those nuances were lost on pharmaceutical marketers newly intent on selling their painkillers to wary doctors. As of June 2017, the Porter and Jick paragraph had been cited 608 times, mostly as evidence that long-term opioid therapy isn’t addictive. (By contrast, 11 stand-alone letters to the journal around the same time were cited a median of 11 times.)
Most of those references appeared after pharmaceutical company Purdue Pharma developed OxyContin in 1995, then reached back 15 years to the Porter and Jick study to claim that the risk of addiction to their new drug was “less than 1 percent.” The company touted OxyContin’s time-release feature—the drug can be taken once every 12 hours, as opposed to taking an immediate-release drug once every 6 hours—as another protection against addiction.
OxyContin brought in $45 million in sales its first year, leaping to $1.1 billion in 2000 and $3.1 billion in 2010, when it had captured 30 percent of the painkiller market.
Johnson & Johnson and Endo Pharmaceuticals joined Purdue in pushing their opioid products as solutions to chronic pain, funding nonprofits that advocated for more pain-pill prescriptions and underwriting continuing-education classes that recommended aggressive pain management. In 2001, based partially on this “emerging and compelling science,” the accreditor Joint Commission told healthcare organizations to better track and alleviate pain, giving the impression that pain—sometimes referred to as the “fifth vital sign”—was being undertreated.
Pain prescriptions shot up, quadrupling from 1999 to 2015, the latest year for which the Center for Disease Control (CDC) has records.
“Previously, opioids had primarily been reserved for severe acute pain, postsurgical pain, and end-of-life care,” the CDC reported. Now, more prescriptions for “chronic noncancer pain” were leading to more long-term prescriptions, which were leading to higher dosages as patients adjusted to their prescriptions and then needed the dose increased.
But just saying a drug isn’t addictive doesn’t make it true, and that soon became obvious. In 2007, Purdue—and three executives—pled guilty to making false claims. Purdue was ordered to pay government and civil claims of more than $634 million. Since then, cities and states have filed dozens of lawsuits against five pain-pill manufacturers for deceptive marketing, looking for payouts to “subsidize substance-abuse programs,” University of Georgia law professor Elizabeth Burch told The Wall Street Journal.
Purdue agreed to pay Kentucky $24 million over OxyContin marketing; Cardinal Health Inc. and AmerisourceBergen settled with West Virginia for $36 million after filling millions of suspicious painkiller orders. “[T]here is blood in the water at this point,” Burch said.
Some believe the opioid lawsuits could swell the way tobacco suits did: In 1998, tobacco companies settled on a $206 billion payout with 46 states.
White and Rural
Most opioid prescriptions are being filled in towns and small cities with white residents, many of whom are unemployed or uninsured, according to the CDC.
“Rural Appalachia has less opportunity for economic or social mobility,” said Kevin Eames, professor of psychology and department chair at Covenant College. He teaches undergraduate- and graduate-level addiction classes.
“Many people depend on coal-mining to survive, which is a dangerous, tedious, and labor-intensive job,” he said. “Poverty tends to produce family dysfunction, which is passed down from generation to generation. A combination of hopelessness, emotional wounds, and physical pain make substance abuse highly likely.”
In addition, doctors may have a faster trigger finger when it comes to scribbling prescriptions for white patients. Studies have reported that black patients receive fewer pain prescriptions, and that some medical students and residents falsely believe black people have a higher pain tolerance.
“We know the challenges related to race and difference are a continued struggle,” said Lloyd Gestoso, dean of the School of Social Work at Cairn University in Pennsylvania. While the undertreating of black pain may have protected more African Americans from opioid addiction, racial issues likely affect how lawmakers and the public have reacted to the opioid crisis differently than to crack cocaine, which ravaged African-American communities in the 1980s.
“Unlike what was heard during the 1980s and 1990s about ‘arrest’ and ‘incarceration’ of those who used crack and other illicit drugs, the word heard today for opioid users is ‘treatment,’” wrote one African-American journalism professor.
“White heroin addicts get overdose treatment, rehabilitation, and reincorporation, a system that will be there for them again and again and again,” law professor Ekow Yankah wrote for The New York Times. “Black drug users got jail cells and ‘Just Say No.’”
The different reactions may also be due to prevalence. More than one in four Americans (27 percent) knows someone who is or has been addicted to opioids; some of them belong to “influential families,” Gestoso said. That familiarity is breeding compassion instead of contempt: Close to seven in 10 Americans said they “understand how someone accidentally gets addicted to opioids,” the American Psychiatric Association reported.
Another difference between opioids and crack cocaine or heroin is the legality. “While opioids like Vicodin are prescribed by a doctor for pain management, crack and heroin are distributed illegally through criminal networks,” Eames said.
Pastoring in America’s Most Addicted State
Predominately white and poor, with small towns and cities, West Virginia is the perfect candidate for opiate addiction.
It didn’t help that drug wholesalers ignored suspicious orders and flooded the state with painkillers. Over six years, wholesalers shipped in enough pain pills for every man, woman, and child to have 433 each. (In one town of 392 people, a single pharmacy ordered 9 million hydrocordone pills over two years.)
So it’s no wonder that West Virginia has the highest overdose rate in the nation.
“Last summer, we had 26 overdoses in four hours in Huntington,” said Chris Priestley, lead pastor at Crossroads Church in Morgantown, about three hours northeast of Huntington. Huntington’s population is about 48,000. “They ran out of ambulances.”
Priestley first ran into opioids when he worked with youth in Charleston. The kids he talked to at the skate parks were using the drugs after they got into a fight, or for a bad report card. Reaching for pain pills “was a consistent pattern,” he said.
Priestley is in Morgantown now, the state’s third-largest city at around 31,000.
“Several members of our congregation have been users in the past or are currently struggling,” he said. “We don’t feel adequate to face this thing. . . . We have the heart but not the means.”
Because opioid addiction is nearly impossible to kick. When someone uses opioids, his or her brain produces more opioid receptors, which feel uncomfortable when they’re empty. And when the brain floods itself with dopamine during opioid hits, it stops producing its normal amount of dopamine. But the body needs that regular dopamine, which makes the craving for opioids even stronger. (The brain changes are even more stark in those whose prefrontal cortex hasn’t yet matured—so anyone younger than 25.)
“It’s the worst stuff ever to try to come off of,” said Donnie Griggs, lead pastor at One Harbor Church in Morehead City, North Carolina. And yet, nobody wants to stay addicted.
“Nobody is proud of it,” Griggs said. One of his family members became addicted through prescribed medication for pain; another began with marijuana and gradually amped up. (“I’m scared of taking anything more than Tylenol,” Griggs said.)
The epidemic reminds Griggs of Isaiah 6, when the prophet laments being among “a people of unclean lips.”
“This isn’t a problem that happens in a big city somewhere, or in another country,” Griggs said. “This happens here, to my friends, my family, my neighbors, my kids. This is our problem. These people feel trapped, addicted, hopeless, ashamed, with no way out. This is here.”
It guts him. “We are drowning in this,” he said. “Everywhere I go, small towns are being eaten up with this stuff.”
Freedom Farm
At Freedom Farm, Quigley helps by bringing everything back to Jesus, over and over again. When he was addicted, he saw Christianity as a standard of morality he’d never be able to meet. (It’s also a standard Freedom Farm itself hasn’t always met. Three years ago, founder Robbie Collie quit amid charges of favoritism and lack of financial transparency. Quigley has also faced criticism.)
The answer for addicts is “the same answer as for you and me,” he said. “Life gets everybody to where they’re feeling trapped. The gospel gives us lenses to look at and interpret life.”
Quigley walks the men through three phases: detox, restoration (residents work through Robert Thune’s Gospel-Centered Life curriculum, learn the physiology of addiction, and get involved at a local church), and discipleship (residents get jobs, attend classes four nights a week, and have regular counseling).
Quigley charges $150 a week, which covers about half the cost of the program. He asks residents to stay for a year, because he thinks that’s how long it takes—at least—to establish good habits and practice living off drugs.
His program is an alternative to some other Christian programs he’s seen—some “revolving doors,” some asking residents to “vomit out the demons,” some so full of strict rules and consequences that the freedom after leaving can catapult people right back into addiction.
“They don’t know what to do,” he said. “Everybody wants results and is trying to produce them.”
Looking for Results
When Jason McClanahan came to Charleston, West Virginia, to re-plant Randolph Street Baptist Church, he ran smack into heroin, meth, and prescription pain pills.
“We became very frustrated in our efforts at discipling and confronting guys,” he said. So five years ago, the church started researching the best ways to help. They asked social workers and law enforcement, doctors and psychologists.
Randolph Street Baptist wanted to address the whole person, “convinced that God created us diverse, complex individuals.” They created Hope for Appalachia, a nonprofit to help men recover from addiction and think through what a Christ-honoring life looks like for them.
Determined to give the men dignity, they purchased and decorated three homes, two next to each other, another two-and-a-half blocks away. That one’s already for sale again—turns out it’s “two-and-a-quarter blocks too far away” for accountability, McClanahan said.
Hope for Appalachia takes men who have been drug-free for at least a month; leaders aim to help relieve the stress that may have driven them to drugs in the first place.
“I’ve been pastoring for 18 years and have never been engaged with something as consuming as this,” McClanahan said. “I was naive going in. I thought, Oh, hey, we’ll help these guys get a couple of things right in their lives and they’ll be okay. It’s so much more than that.”
Every element of the residents’ lives has to be addressed from a Christ-centered perspective, from education to employment to family relationships, he said.
Hope for Appalachia has been around for 18 months, but is already looking to expand. They have room for 12 men but want to double that number, taking in more men, women, and those who haven’t been able to be 30-days free.
“If we took everyone that called us we’d have 50,” McClanahan said. “We have to turn people down weekly.”
But for those who do get in, Hope for Appalachia is with them for life. “Even when they leave us, whether on a good note or a bad one, our commitment is with them long term,” McClanahan said.
Quigley says the same. Men who have graduated from Freedom Farm sometimes relapse after they leave, and sometimes they call him to talk it through.
Those relapses are a common part of recovery, because the drugs make the brain super-sensitive to anything that triggers a craving, Eames said.
“Relapse isn’t a failure, but an event that allows you to learn what went wrong so you don’t make the same mistake again,” he said. He’s optimistic that anyone addicted to opioids can quit.
“For a minority of [users], relapse will be a possible problem for the rest of their lives,” he said. The trouble is, when opioid use becomes an epidemic, the small minority is thousands of people.
What if You Don’t Have a Recovery Center?
Not every church can whip up a recovery center, especially those small churches in rural areas where opioid abuse is most rampant.
“We have to recognize what we can and cannot do,” Priestley said. “I’d love to see a treatment center or a halfway house, but we don’t have the manpower or the expertise or the resources.”
So instead, Priestley aims for preventative care by providing gospel-centered, grace-filled preaching, biblical counseling, and solid pastoral care. His Crossroads Church partners with other organizations and the medical community.
“We want to connect people to care that is comprehensive, while also being present and welcoming them to a new gospel community, so they can hope and heal alongside those who love Jesus,” he said. “We’ve truly seen transformation in those scenarios.”
He connected with a recovered addict over a love of punk rock music, invited him to church, and eventually baptized him. Now, grounded in the Crossroads community, the man invites his friends, who are struggling to join him in freedom from addiction.
“We are not seeing a massive revival or loads of users being healed,” said Priestley, who has worked with about a dozen people struggling with opioid addiction in the past five years. “But we are seeing, through that relationship, people who are coming out of it.”
Communities like the one Priestley is offering are “tremendously effective” support for an addict’s recovery, Eames said.
Sam Quinones, who dug into the opioid crisis in his award-winning 2015 book Dreamland, would likely say the same thing. “This is a story about isolation versus community, really,” he told EconTalk. “It seems to me that a drug that is created and thrives on isolation, that the way to attack it is defeating it through community.”
Churches can also play a key role in relieving the underlying stressors—financial, relational, spiritual, physical—that may send a person to opiates in the first place.
Priestley doesn’t preach explicitly about drugs, but “woven into any gospel message is a call to surface—in other words, to make yourself known. . . . We’re going to walk alongside you, whether you’re struggling with sexual immorality or addiction or pride.”
Griggs names it right out. “When we talk about our town’s brokenness, we put a name on it. We talk about the pill addiction.”
Naming the problem seems to encourage people to come forward to ask for help, though the shame is deep, and extra complex for those whose addictions grew out of legitimate doctor’s prescriptions.
“‘My doctor said I needed this’—I hear that so much,” Griggs said. They aren’t potheads, but soccer moms and well-dressed grandparents and working professionals. “For a soccer mom to go to the hospital and say, ‘I’m addicted to Oxycontin or heroin’—there’s a stigma in our town. And we have only one hospital for our whole county. She knows all the people [working] at the hospital. . . . People really feel trapped.”
That may be part of the reason why “it feels like we are doing more funerals for people than seeing people come out of it,” he said.
Eight years ago, Griggs formed a relationship with the funeral home, and has been conducting funerals for unchurched people who overdosed. “I feel like I’ve talked about the gospel in front of every drug dealer multiple times,” he said. “You don’t get much of a better chance than at a funeral to stand up and talk to a room of people who are addicted to drugs about the hope of Jesus.”
Worth It
Wading into the opioid flood can be heartbreaking and discouraging. Progress is slow and riddled with relapses.
Griggs’s team “pray and pray and pray, and our calendars are filled up with trying to help people,” he said. “I don’t think we feel paralyzed. I think we feel that we have to do something—we can’t not do something. And we also feel like everything we’re doing isn’t enough.”
McClanahan knows that tension.
“Do you know how many times I’ve wanted to quit? . . . Addicts absorb a lot and give back very little,” he said. “But there are few things more addicting—forgive the use of that word—than seeing the work of Christ in a man who had no hope. That one life that you see transformed by the gospel is so worth it in light of the other disappointments and discouragements.”
When God works in a person whose everyday life was “prostitutes and addiction and stealing from others . . . it’s like a gem on a black cloth. It shines so brightly,” he said. “At times you can see the work of Christ in them more clearly because of the darkness of their background.”
McClanahan got to watch a now-employed father open up a 529 plan for his 7-year-old daughter. He got to see a young professional find his way past guilt and shame to finally meet his eyes when they talk. And he got to see a 26-year-old—who had been using for 13 years—get his driver’s license for the first time.
“Man, if you coulda seen the smile on his face,” McClanahan said.
Quigley is still riding the high of a former resident’s recent wedding. “Everything we talked about was Christ-centered, even though it had been years” since they’d seen each other, Quigley said. “His wedding ceremony was a gospel presentation.”
Theology of Addiction
Addiction—and its mental, emotional, and physical affects—is a sign of our total depravity, McClanahan said. “As a result of the fall, we are all sinners, and all of us sin differently, whether drugs or pornography or anger or pride.”
Opioid addiction is both simply sin and also a lot messier than that. The claws of its addiction are especially long and sharp, and often sink in through the innocence of a doctor’s prescription.
“I’ve seen a lot of good people who love Jesus get hooked on this stuff,” Griggs said. In addition, “a lot of people are taking their hopelessness to this instead of the cross. This has been prescribed as a way to deal with pain and sadness, because I don’t think the church has done a great job of explaining how the gospel encounters us in suffering and mourning. The church has almost made it sound like if you aren’t smiling all the time, something is wrong with your Christianity.”
But the church also has the right answer. Along with providing presence and support, it can point addicts to the only solution for sin.
“Addicts are not immune from the hope of the gospel,” Priestley said. “That’s pretty important to remember, to stay grounded instead of getting overwhelmed. I’m called to preach the gospel—that’s not irrelevant to my city’s crisis. That actually applies. . . . We have every reason—because of the cross and the resurrection—to have hope for the future.”
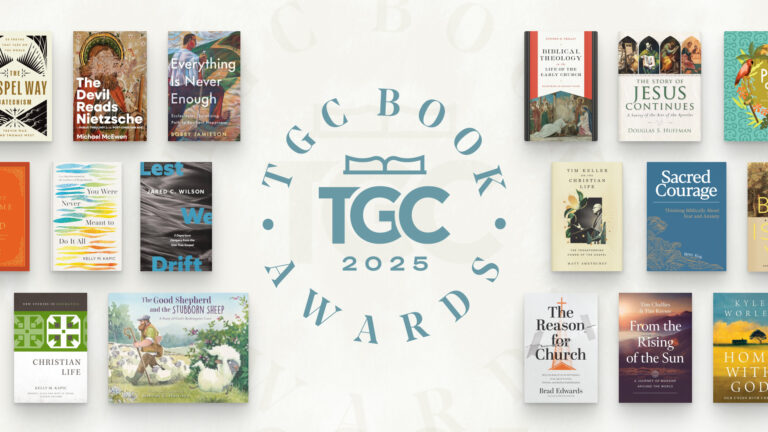
Download your free Christmas playlist by TGC editor Brett McCracken!
 It’s that time of year, when the world falls in love—with Christmas music! If you’re ready to immerse yourself in the sounds of the season, we’ve got a brand-new playlist for you. The Gospel Coalition’s free 2025 Christmas playlist is full of joyful, festive, and nostalgic songs to help you celebrate the sweetness of this sacred season.
It’s that time of year, when the world falls in love—with Christmas music! If you’re ready to immerse yourself in the sounds of the season, we’ve got a brand-new playlist for you. The Gospel Coalition’s free 2025 Christmas playlist is full of joyful, festive, and nostalgic songs to help you celebrate the sweetness of this sacred season.
The 75 songs on this playlist are all recordings from at least 20 years ago—most of them from further back in the 1950s and 1960s. Each song has been thoughtfully selected by TGC Arts & Culture Editor Brett McCracken to cultivate a fun but meaningful mix of vintage Christmas vibes.
To start listening to this free resource, simply click below to receive your link to the private playlist on Spotify or Apple Music.